More Information
Submitted: March 18, 2022 | Approved: June 27, 2022 | Published: June 28, 2022
How to cite this article: Agarwal S, Agarwal S, Verma RK, Dayal S. Clinical profile, etiology, outcome and new-onset diabetes: A SARI case series. J Clin Intensive Care Med. 2022; 7: 005-015.
DOI: 10.29328/journal.jcicm.1001041
Copyright License: © 2022 Agarwal S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Clinical profile, etiology, outcome and new-onset diabetes: A SARI case series
Siddharth Agarwal* , Sapna Agarwal, Raj Kumar Verma and Shreyash Dayal
, Sapna Agarwal, Raj Kumar Verma and Shreyash Dayal
Department of Physiology and Medicine, Faculty of Integrated Medicine, Saran Ashram Hospital, Dayalbagh Educational Institute, Dayalbagh, Agra 282005, India
*Address for Correspondence: Dr. Siddharth Agarwal, MD, Professor, Department of Physiology and Medicine, Faculty of Integrated Medicine, Saran Ashram Hospital, Dayalbagh Educational Institute, Dayalbagh, Agra 282005, India, Email: [email protected], [email protected]
Introduction: The world is currently facing the SARS-CoV-2 pandemic with evolving 2nd wave. The COVID-19 patients present most commonly with Severe Acute Respiratory Illness (SARI) in an emergency room with acute onset fever, cough, and breathlessness. However, not all SARI cases as per definition are due to COVID-19 infection, which is well proven in this case series of 113 cases of SARI. This is just the opposite of the other SARI series done in the pre-COVID-19 era. Also, no previous SARI case series data has shown significant association with Diabetes Mellitus, including new-onset diabetes thus figuring out the major Pathophysiological association of COVID-19 with glucose metabolism and has a bearing on the pathogenesis, treatment, and outcome of COVID-19 infection and perpetuity of pandemic of this magnitude. Here we raise concern for the first time about the growing association of an infectious pandemic with the lifestyle disorders which are non-communicable diseases but carry with them the potential of fertile soil for rapidly spreading epidemics.
Aim and objective: To find out the etiology, clinical profile, treatment outcome, and mortality rate in different sub-groups of SARI cases in a tertiary care hospital and the incidence of new-onset Diabetes Mellitus in them and to investigate theoretically the hypothesis that maintaining normal glucose metabolism could prevent progression of a mild Flu-like illness (FLI) to a severe form of Severe Acute Respiratory Illness (SARI) and consequent complications such as Cytokine Storm Syndrome and Multi-Organ failure.
Design: Retrospective, single-center case series of 113 SARI patients at a tertiary care hospital in Agra India between 1 March- 30 October 2020.
Main outcome: The demographics, clinical, pathological, imaging, and treatment outcome data were collected. The SARI cases analyzed were defined as “Severe acute respiratory infections (SARIs) an acute respiratory illness of recent onset (within seven days) manifested by fever (≥38°C), cough and shortness of breath or difficulty in breathing requiring hospitalization and were sub-classified according to the primary etiology producing SARI in them. The findings were compiled and compared.
Conclusion: Of the 113 patients of SARI – 32.7%were associated with Diabetes, with 9.74% new-onset Diabetes and 26% previously known Diabetes. This was mainly due to SARS-CoV-2 (24 Diabetics out of 52 COVID-19 cases- 46.1%).
The Average hospitalization stay of SARI cases was 10 days with a maximum in SARS-CoV-2 and a minimum stay of 5.22 days in Bacterial Pneumonia and 5.66 days in Koch’s Lungs.
The death rate was maximum (4 out of 26) 15.3%. Hospitalized TB/Koch’s Lung patients who presented as SARI and 3.8% in Bacterial Pneumonia, 2.43% in SARS-CoV-2, and <1% in Sepsis.
Those SARI cases who were euglycemic at the time of initial presentation recovered early and carried a good prognosis with less mortality as compared to those who were hyperglycemic on presentation. Also, those FLI cases who maintained euglycemia or did not have any other risk factor which predisposes them to stress (Diabetes, Prolonged fasting, Obesity, major organ disorder, Psychological disorder, and Cancer) did not progress to SARI as the endogenous steroid secretion and sympathetic activation did not occur, the intracellular pH levels remained in the alkaline range.
10.18% of cases developed new-onset diabetes (a total of 11 cases) out of which 10 were in COVID-19. Thus 19.2% incidence of new-onset diabetes in SARS-CoV-2 and a prevalence of 26.9% in SARS-CoV-2, making total diabetes 46.1% in SARS-CoV-2, and out of all SARI cases, 26% of patients developed pulmonary fibrosis with consequent long-term complications. In COVID-19 patients, it was seen only in diabetics SARS CoV-2 male patients, thus no death in non-diabetic females in COVID-19 in this case series.
As per WHO recommendation, surveillance is required for hospitalized severe acute respiratory infection (SARI) cases, and influenza-like illnesses (ILI) cases outpatient [1-3].
This has been conducted in many nations for the last few years but with the advent of the SARS-CoV-2 pandemic, the pre-COVID-19 era data has to be revised to effectively constitute new policy arising out of the lessons learned during this COVID-19 pandemic. The role of Coronavirus and other bacterial infections including mycobacterium tuberculosis (TB) presenting as severe acute respiratory illness and carrying variable morbidity and mortality needs proper documentation with the available data. Tuberculosis is also an important cause of severe respiratory illness (SRI) presenting acutely and causing significant morbidity and mortality globally. In 2015, an estimated 10.4 million people developed tuberculosis and 1.8 million died from the disease [4]. In 2019, an estimated 10 million people fell ill with tuberculosis (TB) worldwide. 5.6 million men, 3.2 million women, and 1.2 million children. TB is present in all countries and age groups. TB is curable and preventable [5].
The emerging role of Diabetes Mellitus in modifying the clinical profile and treatment outcome in SARI cases also needs to be studied thoroughly [6], as experienced in the COVID-19 pandemic, where new-onset diabetes mellitus was diagnosed as naïve cases in COVID-19 positive patients. There is a bidirectional relationship between COVID-19 and diabetes. On the one hand, diabetes is associated with an increased risk of severe COVID-19, while on the other, new-onset diabetes and severe metabolic complications of preexisting diabetes, including diabetic ketoacidosis and hyperosmolarity for which exceptionally high doses of insulin are warranted, have been observed in patients with COVID-19.1-3 These manifestations of diabetes pose challenges in clinical management and suggest complex pathophysiology of COVID-19–related diabetes [7-9].
In this current study, the surveillance data of hospitalized SARI patients in a tertiary care hospital were analyzed from 15 March-30 October 2020 to identify various sub-groups of infections causing SARI, their clinical profile, the outcome of treatment, and mortality rate too, address the community-based approach in dealing with SARI cases, thereby reducing the morbidity and mortality and also to assess the impact of emerging new-onset diabetes mellitus as a chronic metabolic disorder in the causation, outcome, and management of pandemics of this magnitude.
The world is currently facing the SARS-CoV-2 pandemic with evolving 2nd wave, which originated in Wuhan China in December 2019 [10]. To date 111 million [11] of the world population have been infected with the novel coronavirus and 2.4 million have died due to it. The COVID-19 patients present most commonly with Severe Acute Respiratory Illness (SARI) in an emergency room with acute onset fever, cough, and breathlessness. As per WHO, the case definition of Severe Acute Respiratory Infections (SARI) is anyone with acute respiratory infection with symptoms within 10 days of presentation, cough, fever, and hospitalization [12]. However, not all SARI cases as per definition are due to COVID-19 infection, which is well proven in this case series of 113 cases of SARI. This is just the opposite of the other SARI series done in the pre-COVID-19 era. Sentinel surveillance among severe acute respiratory illness (SARI) patients can help identify the spread and extent of transmission of coronavirus disease 2019 (COVID-19). SARI surveillance was initiated in the early phase of the COVID-19 outbreak in India also [13].
Several studies have identified an increased risk of severe disease in SARS-CoV-2 infection who have other co-morbidity like obesity, hypertension, chronic lung disease, diabetes mellitus, Psychological disorders, cancer, and cardiovascular disease. But no previous SARI case series data has shown a significant association between COVID-19 infection-causing new-onset diabetes mellitus. Thus, the major Pathophysiological association of COVID-19 with glucose metabolism has a bearing on the pathogenesis, treatment, and outcome of COVID-19 infection. These observations and several in-depth reviews [14] have figured out the metabolic syndrome with impaired glucose metabolism as a major prognostic factor in severe COVID-19 infections.
We report here our experience of 113 patients admitted as SARI cases in a tertiary care hospital in Agra, India within the epicenter of the SARS-CoV-2 pandemic in India. This case series points out that many causes present as SARI, with SARS-CoV-2 as only one of them. In this pandemic, the causes of SARI other than SARS-CoV-2 are being overlooked and not receiving the medical attention as per need. Hence the mortality rate in them is also more than the mortality rate of SARI due to COVID-19. Here we also raise concern for the first time about the growing association of an infectious pandemic with the lifestyle disorders which are non-communicable diseases but carry with them the potential of fertile soil for rapidly spreading epidemics. The significant association of new-onset diabetes In COVID-19/SARI cases opens up a new era of hybrid disorders which we label the germ theory of Diabetes mellitus.
The current case series of SARI patients carried out over a period from 15 March to 31 October 2020 of 113 patients at a tertiary care hospital was done with the following aims and objectives.
1. To find out the cause of SARI cases hospitalized in a tertiary care hospital. The period in observation was a focused era of the COVID-19 pandemic and almost all, medical and health facilities in the world were tackling the SARS-CoV-2 pandemic. However, we aimed to find out the exact proportion of SARI cases due to SARS-CoV-2 and also to know the other causes presenting as SARI like bacterial pneumonia, sepsis causing respiratory failure, acute infection in COPD cases, and Tuberculosis presenting as an acute respiratory infection.
2. The mortality rate among the different sub-group of SARI. The more focused approach on SARS-CoV-2 patients with a global mortality rate of 1.2 per million and a case fatality rate of India 1.5% seems to be much less or equal to the mortality rate of other SARI sub-groups. This is a very important factor in the management of SARI cases carrying a high mortality rate than SARS-CoV-2.
3. The age range of the population suffering most from SARI as well as the age range of SARI cases having maximum mortality is compiled in this SARI case series data. This observation will let us know which age is more susceptible to SARI and the reasons for it. Further what intervention can be done as a protective measure in the particular age range to reduce morbidity and mortality will be our future direction.
4. The presence of co-existing co-morbidity like Diabetes Mellitus, hypertension, heart disease, cancer, other systemic illness, and obesity in the SARI cases and their impact on the outcome of management of different SARI sub-groups is another aim of this study. Particular significance is laid on a disorder of glucose metabolism manifesting as Diabetes Mellitus, as the preventive literature and the latest observations from different case series have shown that diabetes and obesity carry poor prognosis in SARS-CoV-2 patients. Here we would also like to find out the reason for the above association if any and our observation for further exploration that by maintaining normal glucose metabolism in the ongoing pandemic we could prevent the progression of the mild flu-like illness (FLI) to SARI.
5. Do initial interventions in the outpatient department (OPD) on a patient presenting as FLI could protect their progress to SARI and or sub-group complications, irrespective of the cause of FLI in a current scenario of global emergency. Here we aim to know the impact of our oral dexamethasone in a dose of 3 ml/day (adult). Given FLI cases in the OPD and to see its impact as compared to the controlled group who were not given dexamethasone. This observation has been attempted from the finding which was seen in the Victoria trial. We propose to further conduct a randomized controlled trial on this observation as a further direction.
6. Knowing the incidence of new-onset of diabetes mellitus in different SARI sub-groups and fit is significantly associated with their doses it supports the germ theory of diabetes.
Study population
In a tertiary care hospital in the city of Agra. The patients of all ages of both series were admitted to the hospital with Severe Acute Respiratory Infection (SARI) as per the WHO definition, from 2 March 2020 to 31 Oct 2020.
The patients were labeled as SARI as per the definition of WHO. There was no age and sex bar in this case series. The admitted patients of SARI were evaluated for the causeproducing immediate Severe Acute Respiratory Illness and any associated co-morbidity like Diabetes, Hypertension, Morbid Obesity, Kidney disease, Liver disease, Heart disease, major psychological disorders, and Cancer.
The COVID-19 testing was done by both antigen and antibody-based tests. The sputum was tested for culture and sensitivity. The imaging test done were chest X-rays and CT scans of the thorax. The glycosylated hemoglobin and fasting, as well as post prandial sugar levels of all participants, were recorded besides other routine hematology, biochemistry, and serology tests. The consent for the participation was obtained from all subjects. This was purely an observational study without any study-based intervention. So, there was no control group. The study was done on a group of Cohorts who share common characteristics of presenting as Severe Acute Respiratory Illness.
Ethical standard
Before study initiation, the study protocol was approved by the intuitional review board in compliance with the central trial registry of India and informed consent was from obtaining from the patient /guardian. All relevant ethical guidelines have been followed. Details of the oversight body: SIDDHARTHA HOSPITAL INSTITUTIONAL REVIEW BOARD Approval date: 05/05/2020 Reference No: CRT/05/01. Oversight body that provided approval to IRB: Department of Health Research, Ministry of Health and Family Welfare, Government of India, National Ethics Committee Registry for Biomedical and Health Research (NECRBHR). All necessary patient/participant consent has been obtained. The clinical trial involved has been registered with an ICMJE-approved registry. The clinical trial ID is CTRI/2020/05/02540 and UTN No is U1111-1252-7438. Global case surveillance protocol was followed for SARI cases and include Acute Respiratory infection with a history of fever or measured fever more than 38⁰C and cough with onset within the last 10 days and needing hospitalizing. The collected data from the enrolled patient includes the patient’s demographic medical history, clinical signs, and symptoms, Co-morbidities, treatment given, clinical course, and outcome. The investigation done include nasopharyngeal and oropharyngeal swabs for detecting Bacteria, virus, and macrobacterium tuberculosis on admission. Also, the IgM and IgG antibodies for SARS-CoV-2 in the patient’s blood were screened.
Main outcome and results
The demographics, clinical, pathological, imaging, and treatment outcome data were collected. The SARI cases analyzed were defined as “Severe acute respiratory infections (SARIs) an acute respiratory illness of recent onset (within seven days) manifested by fever (≥ 38 °C), cough and shortness of breath or difficulty in breathing requiring hospitalization and were sub-classified according to the primary etiology producing SARI in them. The findings were compiled and compared.
The above data table shows the characteristics of 113 cases of this SARI case series, with their date of initial presentation, age, presenting symptoms, diagnosis, co-existing disorders, and outcome Table 1.
| Table 1: Patients Characteristics. | |||||
| S.No | Date | Age | Symptoms | Diagnosis | Outcome |
| 1 | 11-Oct | 26/M | Fever, Cough | TB Lungs | Improved |
| 2 | 62/M | Fever, Cough, SOB | Covid-19, Diabetes, Hypertension | Improved | |
| 3 | 14-Oct | 60/M | Fever,Cough,SOB, Chest Pain | Right Lung Pneumonia | Improved |
| 4 | 20-Oct | 52/F | Fever, Cough | Covid-19 | Improved |
| 5 | 21-Oct | 65/M | Dyspnea, Sweating, Chest pain | Bi-fascicular Block | Improved |
| 6 | 25-Jun | 55/M | Dyspnea, Cough | LLZ Pneumonia, | Improved |
| 7 | 30-Jun | 35/M | Chest pain,Cough,Fever | Right Pleural Effusiun | Improved |
| 8 | 26-Sep | 35/F | Pain Abdomen,Fever | Pneumonia , Covid-19, New-Onset Diabetes | Chronic Pulmonary Fibrosis |
| 9 | 10-Jun | 65/M | Fever, Dyspnea | Bacterial Pneumonia | Improved |
| 10 | 14-Jul | 28/M | Fever, Dyspnea | Bacterial Pneumonia | Improved |
| 11 | 27-Sep | 54/M | Fever, Cough | Pneumonia, Covid-19 | Chronic Pulmonary Fibrosis |
| 12 | 16-Oct | 50/M | Fever, SOB | Post-TB Sequeal, COPD, Koch's Lung | Chronic Pulmonary Fibrosis |
| 13 | 16-Aug | 57/M | Fever,Cough,SOB, Chest Pain | Pneumonia, Covid-19 | Improved |
| 14 | 30-Sep | 77/F | Fever,Cough,Dyspnea | Pneumonia, Covid-19, New-Onset Diabetes, HTN | Improved |
| 15 | 19-Jun | 55/M | Fever,Cough | Lt.Lower Bacterial Pneumonia, TB, Diabetes | Chronic Pulmonary Fibrosis |
| 16 | 03-Jul | 22/M | Fever, Cough | TB Lungs | Improved |
| 17 | 11-Apr | 37/M | Fever, Cough | TB Lungs | Improved |
| 18 | 29-Sep | 60/M | Dyspnea,Hypoxia | Pneumonia, Covid-19,HTN | Chronic Pulmonary Fibrosis |
| 19 | 10-Sep | 52/M | Fever | Pneumonioa, Covid-19 | Improved |
| 20 | 12-Sep | 57/M | Fever,Cough | Pneumonia, Covid-19, New-Onset Diabetes,HTN | Improved |
| 21 | 12-Oct | 18/F | Fever, Cough | Koch's Lung, Dengue Fever | Chronic Pulmonary Fibrosis |
| 22 | 12-Oct | 55/M | Fever, Cough | Covid-19, New-Onset Diabetes, Hypertension | Improved |
| 23 | 11-Oct | 56/M | Fever,Cough,Dyspnea | Covid-19 | Improved |
| 24 | 08-Oct | 55/M | Fever,Cough,Dyspnea | Koch's Lung | Death |
| 25 | 03-Oct | 50/M | Fever, Cough | Covid-19, Diabetes | Chronic Pulmonary Fibrosis |
| 26 | 02-Oct | 72/M | Fever | Covid-19, Diabetes | Death |
| 27 | 29-Sep | 55/M | Fever,Cough | Bacterial Pneumonia, Diabetes | Improved |
| 28 | 24-Sep | 49/M | Hypertension | Covid-19, New-Onset Diabetes , HTN | Chronic Pulmonary Fibrosis |
| 29 | 25-Sep | 75/M | Fever,Cough | Covid-19, Diabetes | Improved |
| 30 | 20-Sep | 65/M | SOB,Cough | COPD, Koch's Lung | Chronic Pulmonary Fibrosis |
| 31 | 15-Sep | 51/M | Low BP | Covid-19 | Improved |
| 32 | 15-Sep | 18/F | Fever | Covid-19 | Improved |
| 33 | 13-Sep | 40/M | Fever,Cough,Dyspnea | Koch's Lung, Pyo Pneumothorax | Death |
| 34 | 11-Sep | 57/M | Cough, SOB, Chest Pain | Bacterial Pneumonia, Diabetes, IHD | Improved |
| 35 | 30-Aug | 70/M | Fever,Cough | Bi-Lateral Atypical Pneumonia, New-Onset Diabetes, Covid-19 | Improved |
| 36 | 25-Aug | 94/M | Fever | Atypical Bacterial Pneumonia, Diabetes | Chronic Pulmonary Fibrosis |
| 37 | 23-Aug | 63/M | Fever | Bacterial Pneumonia, Diabetes | Improved |
| 38 | 24-Aug | 42/M | Chest Pain | Bacterial Pneumonia, Diabetes | Improved |
| 39 | 21-Aug | 14/F | Respiratory Failure | Koch's Lung | Death |
| 40 | 17-Aug | 50/M | Fever,Cough,SOB | Covid-19 | Improved |
| 41 | 14-Aug | 40/M | Fever | Koch's Lung | Improved |
| 42 | 01-Aug | 79/M | Hypoxia | Bacterial Pneumonia With Sepsis | Death |
| 43 | 27-Jul | 32/M | Cough, SOB, Chest Pain | TB Lungs, Pleural Effusion | Improved |
| 44 | 10-Jun | 80/M | Fever, Dyspnea | Covid-19, Diabetes | Improved |
| 45 | 03-Sep | 57/F | Fever,Cough | Pneumonia, Covid-19 | Improved |
| 46 | 04-Jul | 32/M | Chest Pain, Cough | Rt. Lower Bacterial Pneumonia | Improved |
| 47 | 28-Sep | 50/M | Fever | Pneumonia, Covid-19 | Improved |
| 48 | 13-Sep | 40/M | Fever,Cough | Pneumonia, Covid-19 | Chronic Pulmonary Fibrosis |
| 49 | 11-Oct | 58/M | Fever | Covid-19 | Improved |
| 50 | 12-Sep | 18/M | Fever,Cough | Pneumonia, Covid-19 | Improved |
| 51 | 05-Jun | 59/M | Pneumonia, Covid-19 | Developed malignancy | |
| 52 | 17-Oct | 55/F | Chest Pain, Cough , Anosmia | Bacterial Pneumonia | Improved |
| 53 | 19-Oct | 48/M | Fever, Anosmia | Bacterial Pneumonia | Improved |
| 54 | 25-Sep | 17/M | Fever, Cough | Dengue | Improved |
| 55 | 01-May | 41/F | Cough, SOB, Chest Pain | Asthama, LRTI | Improved |
| 56 | 14-Apr | 18/M | Koch's Lung | Improved | |
| 57 | 09-Jun | 40/M | Covid-19 | Improved | |
| 58 | 02-Jun | 76/F | Bacterial Pneumonia, Diabetes, Ketoacidosis,HTN | Improved | |
| 59 | 18-May | 18/F | Koch's Lung , Anemia | Improved | |
| 60 | 17-May | 20/M | B/L Koch's Lung | Improved | |
| 61 | 09-May | 39/M | Bacterial Bacterial Pneumonia | Chronic Pulmonary Fibrosis | |
| 62 | 26-Apr | 19/M | Hypoxia | CHD | Improved |
| 63 | 25-Apr | 37/M | Pleural Effusion | Improved | |
| 64 | 12-Apr | 72/M | Bacterial Pneumonia, Sepsis, Renal Failure | Improved | |
| 65 | 12-May | 65/F | Fever | Sepsis, Renal Failure, Stoke | Improved |
| 66 | 09-May | 50/M | Liver Failure, IHD, Jaundice | Death | |
| 67 | 04-Apr | 25/F | Fever, Cough | Rt. Bacterial Pneumonia | Improved |
| 68 | 31-Mar | 52/M | Bacterial Bacterial Pneumonia | Improved | |
| 69 | 29-Mar | 50/M | Koch's Lung | Improved | |
| 70 | 28-Mar | 60/F | Koch's Lung, Diabetes | Improved | |
| 71 | 26-Mar | 21/M | Bacterial Bacterial Pneumonia | Improved | |
| 72 | 23-Mar | 38/M | Bacterial Pneumonia | Improved | |
| 73 | 22-Mar | 35/M | Koch's Lung | Chronic Pulmonary Fibrosis | |
| 74 | 20-Mar | 70/F | Bacterial Pneumonia | Chronic Pulmonary Fibrosis | |
| 75 | 20-Mar | 42/M | Pulmonary TB | Death | |
| 76 | 18-Mar | 50/M | Bacterial Pneumonia, COPD | Improved | |
| 77 | 18-Mar | 42/F | Bacterial Pneumonia, Asthama | Improved | |
| 78 | 17-Oct | 60/M | B/L Pneumonia, New- onset Diabetes, Covid-19 | Chronic Pulmonary Fibrosis | |
| 79 | 11-Oct | 42/M | New-Onset Daibetes, Covid-19 | Improved | |
| 80 | 17-Mar | 15/F | Hypoxia | Koch's Lung | |
| 81 | 05-Oct | 55/F | Fever, Pain Abd. | Covid-19 | Improved |
| 82 | 29-Sep | 80/M | Diabetes, Dementia, Covid-19, Hypertension | Chronic Pulmonary Fibrosis | |
| 83 | 12-Oct | 50/M | Valvular heart disease, low EF | Improved | |
| 84 | 16-Oct | 21/M | Dengue Fever, New-Onset Diabetes | Improved | |
| 85 | 16-Oct | 46/F | Dengue Fever | Improved | |
| 86 | 11-Oct | 23/M | Dengue Fever, Covid-19 | Improved | |
| 87 | 11-Oct | 52/F | Dengue Fever, Covid-19 | Improved | |
| 88 | 23-Sep | 24/M | Dengue Fever | Improved | |
| 89 | 02-Mar | 69/M | Diabetes, COPD, Sepsis, Hypertension | Death | |
| 90 | 19-Oct | 51/F | Covid-19 | Improved | |
| 91 | 06-Jul | 32/M | Fever, Cough | Covid-19 | Improved |
| 92 | 15-Jun | 35/F | Fever, Cough | Covid-19 | Improved |
| 93 | 22-Sep | 50/M | Fever, Cough | Koch's Lung | Chronic Pulmonary Fibrosis |
| 94 | 02-Mar | 18/M | Koch's Lung | Chronic Pulmonary Fibrosis | |
| 95 | 17-Mar | 50/M | Acute Myocardial Infarction | Improved | |
| 96 | 20-Mar | 60/F | Diabetes, COPD | Improved | |
| 97 | 14-Sep | 43/M | Covid-19. New-Onset Diabetes | Improved | |
| 98 | 26-Oct | 62/M | Anosmia | Covid-19, Diabetes | Improved |
| 99 | 26-Oct | 65/F | Covid-19, Diabetes | Improved | |
| 100 | 26-Oct | 42/M | Interstitial Pneumonia, Diabetes, Covid-19, Morbid Obesity | Chronic Pulmonary Fibrosis | |
| 101 | 26-Oct | 68/M | Covid-19, New-Onset Diabetes | Improved | |
| 102 | 27-Oct | 60/M | Diabetes, Covid-19 | Improved | |
| 103 | 27-Oct | Dengue, Covid-19 | Improved | ||
| 104 | 05-Sep | 75/M | Diabetes, Covid-19, Hyeprtension | Improved | |
| 105 | 05-Sep | 70/F | Covid-19 | Improved | |
| 106 | 25-Sep | 62/M | Diabetes, Covid-19 | Improved | |
| 107 | 21-Oct | 18/M | Covid-19, Leukemia | Improved | |
| 108 | 25-Oct | 38/M | Fever | Covid-19 | Improved |
| 109 | 27-Oct | 55/M | Diabetes, CLD portal HTN, B/L Pneumonia, Covid-19 | Improved | |
| 110 | 29-Oct | 38/M | Covid-19 | Improved | |
| 111 | 31-Oct | 60/F | Covid-19 | Improved | |
| 112 | 30-Oct | 70/M | Hypoxia | ILD with Bacterial Pneumonia, Diabetes | Chronic Pulmonary Fibrosis |
| 113 | 03-Nov | 67/M | Covid-19, Diabetic, IHD,Hypertension | Death | |
The name and other demographics have been omitted for ethical reasons.
Out of a total of 113, 77% were Male and 23% were female, the mean age was 46 years, the mean age in males was 46.37 and in females was 46.69 years.
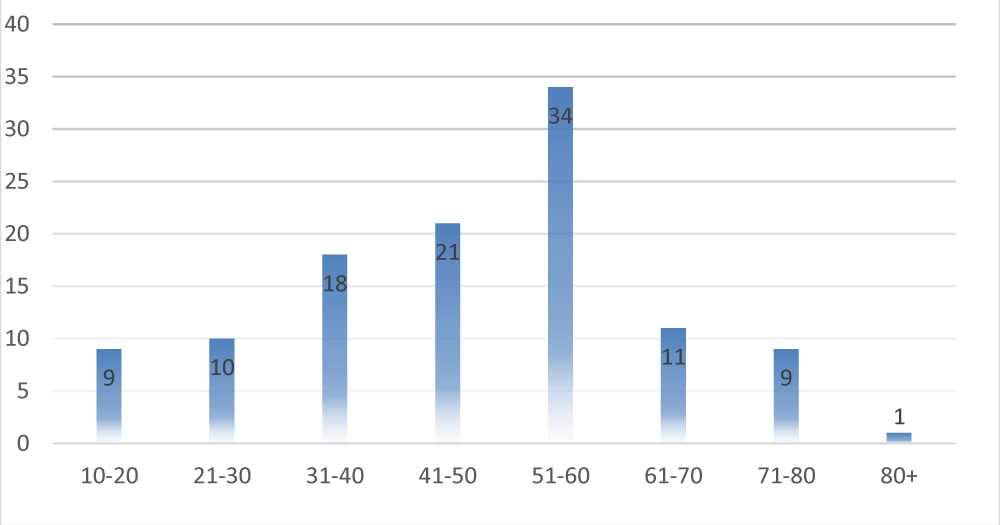
The age range of maximum SARI cases was 51-60 years. See Bar Diagram 1.
Diagram 1: Age Distribution.
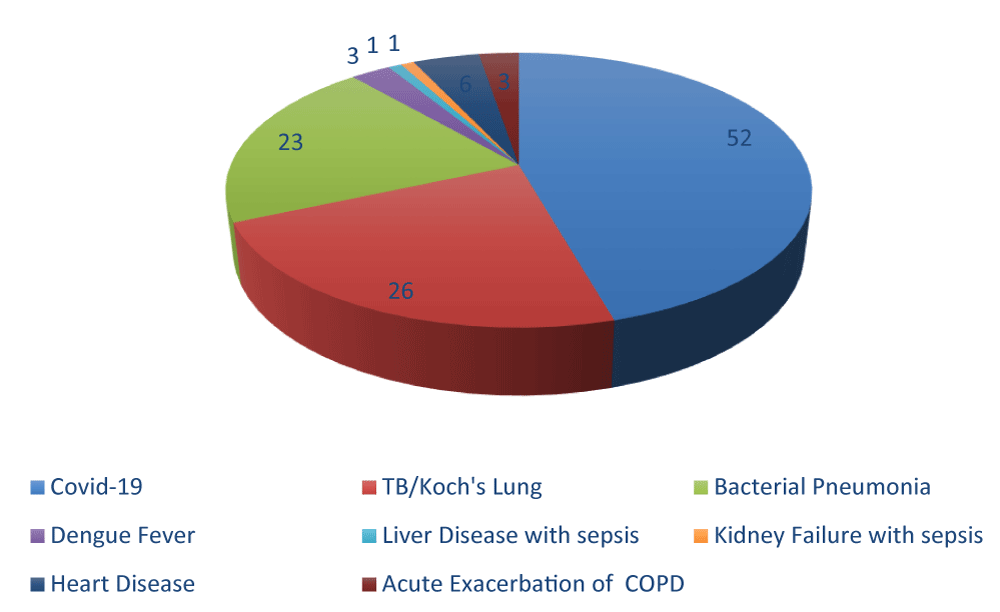
The etiology of SARI cases is shown in Pie Diagram 2.
Diagram 2: Etiology of SARI cases.
About 46% of cases were due to COVID-19 followed by Tuberculosis of the lungs 23%. The bacterial pneumonia was presented as SARI in approximately 20.3%. The acute exacerbation of COPD, Dengue fever, and sepsis were other minor causes of SARI presentation. 4.42% of patients suffering from Heart pathology also presented as SARI with fever, cough, and shortness of breath as primary presentation.
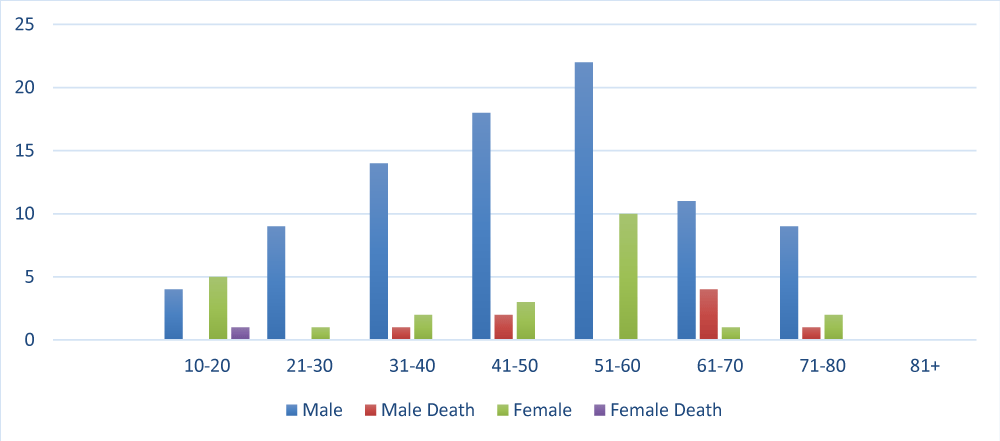
Death was seen more in males (8 out of 87) 9.1% than in females (1 out of 26) 3.8%. Thus, it points out that SARI is more fatal in males, irrespective of the cause. The mortality in COVID-19 patients is 3.8% (2 out of 52) with 5% mortality rates in males versus 0% in females. Thus, we see that COVID-19 carries a bad prognosis in males as compared to females.
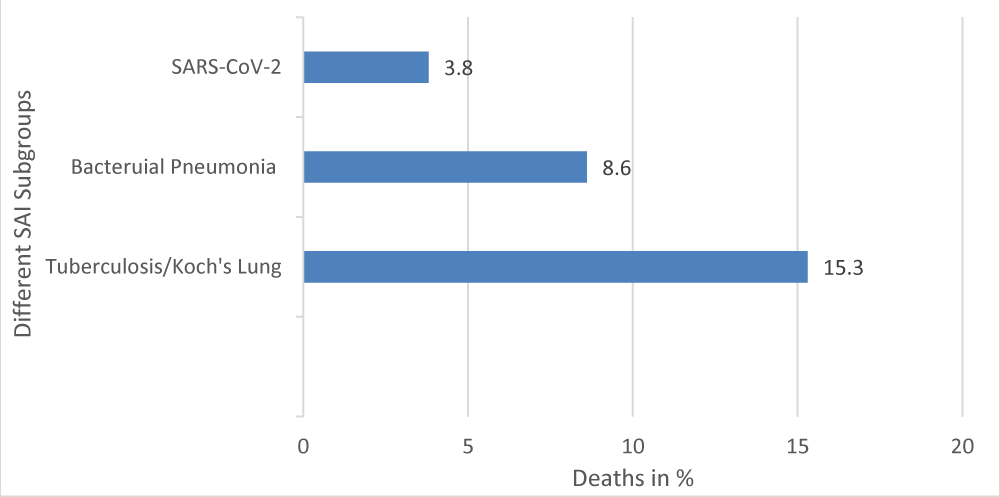
The deaths in TB/Koch’s lung were (4 out of 26), about 15.3%. Thus, the mortality rate of TB/Koch’s Lung is maximum, followed by Bacterial Pneumonia, 8.6%, and then COVID-19, 3.8%. However, the COVID-19 tends to affect males more, both in infection and severity.
The death of Ischemic Heart Disease with SARI due to any infection carries a bad prognosis with 1 death out of 6 subjects (16.66%).
See Bar diagram 3
Diagram 3: Death Age Group Distibution.
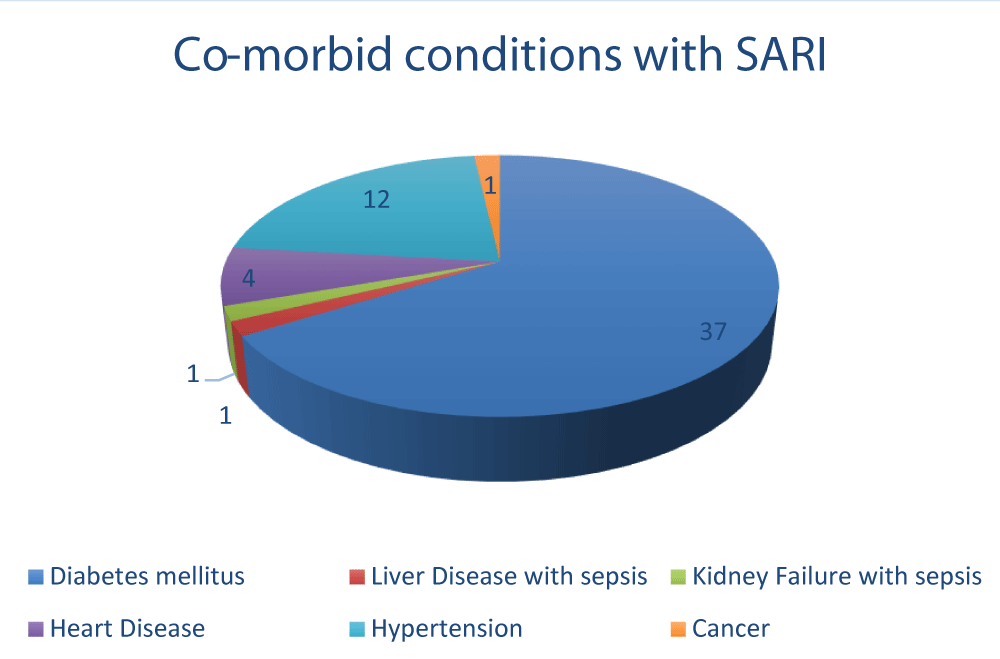
Diabetes mellitus was the most common co-morbid condition associated with SARI patients (32.7%), followed by hypertension (10.6%) and heart disease (5.3%).
Bar diagram showing deaths% in different SARI Subgroups diagrams 4, 5.
Diagram 4: Relation of Deaths in different SARI cases.
Diagram 5: Co-morbid conditions with SARI.
It can be appreciated that 10.18% of cases developed new-onset diabetes (a total of 11 cases) out of which 10 patients were in COVID-19. Thus 19.2% incidence of new-onset diabetes in SARS-CoV-2 and prevalence of pre-existing diabetes in 26.9% in SARS-CoV-2 patients. Making total diabetes 46.1% in SARS-CoV-2. The association of diabetes with bacterial pneumonia was 34.7%. However, the finding of a new onset of diabetes in COVID-19 patients is a unique and significant observation and was persisting up to 3 months observation period after recovery from COVID-19 Tables 2,3.
| Table 2: The number of patients having co-existent different co-morbid conditions along with SARI. | |
| Co-morbid condition | Patients |
| Diabetes mellitus | 37 |
| Liver Disease with sepsis | 1 |
| Kidney Failure with sepsis | 1 |
| Heart Disease | 6 |
| Hypertension | 12 |
| Cancer | 1 |
| Table 3: The incidence and prevalence of New-onset Diabetes and pre-existing diabetes in various SARI subgroups. | ||
| Disease Pre-existing | Diabetes | New-onset Diabetes |
| Bacterial Pneumonia | 8 | 0 |
| Covid-19 | 14 | 10 |
| TB/Koch's Lung | 1 | 0 |
| Dengue Fever | 1 | 1 |
| Liver Disease with sepsis | 0 | 0 |
| Kidney Failure with sepsis | 0 | 0 |
| Heart Disease | 0 | 0 |
| Acute Exacerbation of COPD | 2 | 0 |
The Average hospitalization stay of SARI cases was 10 days with a maximum in SARS-CoV-2 and a minimum stay of 5.22 days in Bacterial Pneumonia and 5.66 days in Koch’s Lungs.
Treatment outcome
It was noticed while treating COVID-19 FLI cases, that those cases who were treated with dexamethasone led to early improvement with non-progression to SARI. A double-blind randomized controlled trial was done on 113 subjects who presented with Flu-like Illness. PISCOV trial approval for the same was obtained from a regulatory authority, the Central Trial Registry of India. The study group received Dexamethasone plus standard care, whereas the control group received standard treatment as per ICMR protocol. The same trial has been completed with results to be published shortly. However, there could be a transient worsening of blood sugar control, particularly in diabetics, but the activation of inflammatory pathway and subsequent progression to Severe Acute Respiratory Illness with cytokine storm was prevented. The raised sugar levels were easily controlled by early tapering of a short course of steroids (used as 3 mg per day of Dexamethasone for 5 days and tapered over the next 5 days) and alongside oral anti-diabetics or transient insulin therapy. The pathways of Glucose metabolism and how it affects the outcome of a simple viral flu presenting as an influenza-like illness to either complete cure or progression to a Severe Acute Respiratory Illness with activation of inflammatory pathways are explained below.
Dysregulated aerobic glucose metabolism leading to progression of mild FLI to SARI
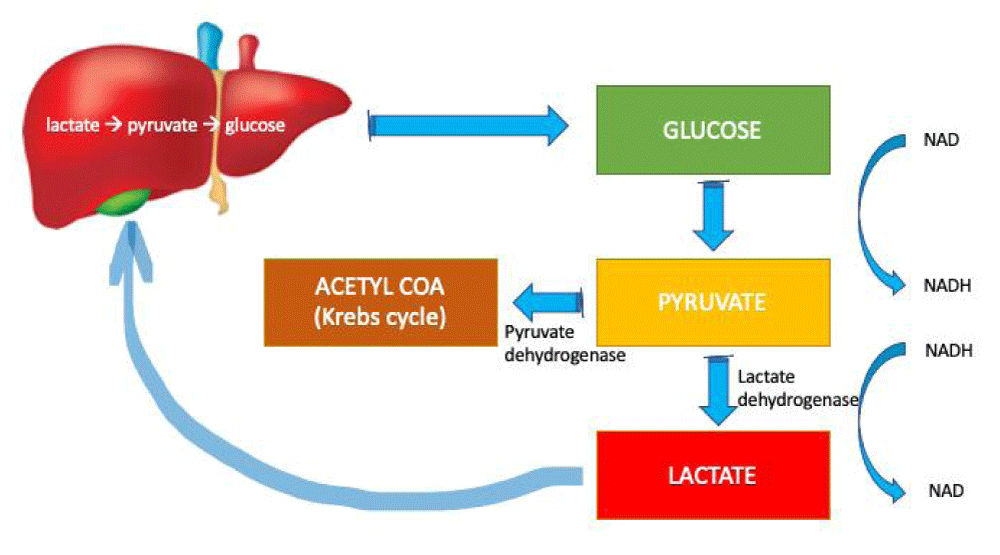
In the glycolytic pathway, glucose is oxidized to pyruvate with the generation of NADH from NAD. The pyruvate is metabolized in the mitochondria by the aerobic pathway through the Krebs cycle. The metabolism of each molecule of pyruvate results in the generation of 36 molecules of ATP. Under anaerobic conditions, the pyruvate does not enter the mitochondria; instead, it is converted to lactate-by-lactate dehydrogenase in the cytosol, with the regeneration of NAD from NADH (Figure 1). The concentrations of lactate and pyruvate are maintained at a 10:1 equilibrium by lactate dehydrogenase.
Figure 1: Normal pathways of glycolysis and gluconeogenesis.
The lactate generated is transported to the liver, where it is oxidized to pyruvate [15]. The pyruvate is converted back to glucose through gluconeogenesis and re-enters the glycolytic pathway (Figure 1). The liver clears 70% of the generated lactate, mainly through gluconeogenesis and partly by oxidation to carbon dioxide and water. Tissues rich in mitochondria, including skeletal and cardiac muscle, and the proximal tubular tubules of the kidney eliminate the remaining lactate by conversion to pyruvate. The kidneys excrete less than 5% of the lactate produced.
Any increase in the rate of glycolysis results in the generation of high levels of pyruvate. The pyruvate dehydrogenase enzyme may be overwhelmed by excessive pyruvate levels; this result, in the conversion of pyruvate to lactate by the lactate dehydrogenase enzyme. Accelerated glycolysis occurs in hypermetabolic states, including fever, thyrotoxicosis, and the use of beta-agonist drugs such as adrenaline.
Here is the main turning point as per our observation and hypothesis. In a patient with mild Flu-Like Illness, if the anaerobic pathway of lactate production is not activated as the body’s glucose is metabolized in a normal Kreb’s cycle via pyruvate generation, do not progress to Severe Acute Respiratory Illness and its LDH (Lactate Dehydrogenase) levels do not rise [16,17].
This is a critical gateway, where we can prevent the progression of FLI to SARI, by regulating normal glucose metabolism.
If, however, the lactate or anaerobic pathway gets activated then the patient’s glucose levels increase due to an increase in gluconeogenesis by the liver and also an increase in glycogenolysis to clear the high production rate of lactate.
Endogenous release of excessive catecholamines or their administration for hemodynamic support may lead to hyperlactatemia through increased activity of the Na+/K+–ATPase pump due to β2-receptor stimulation. This results in cyclic AMP release, with stimulation of accelerated glycogenolysis and glycolysis, leading to excessive pyruvate generation. When pyruvate levels continue to rise, increased conversion to lactate occurs, leading to hyperlactatemia. A hypermetabolic state characterized by excessive release of catecholamines may be the trigger for hyperlactatemia in SARI [18].
Under situations of stress, lactate acts as metabolic fuel through oxidation and conversion to pyruvate and glucose in the liver.
The above explanation is sufficient to support the observation of the high incidence of SARI in COVID-19 patients with diabetes as well as the high incidence of new-onset Diabetes in COVID-19 patients who present as SARI.
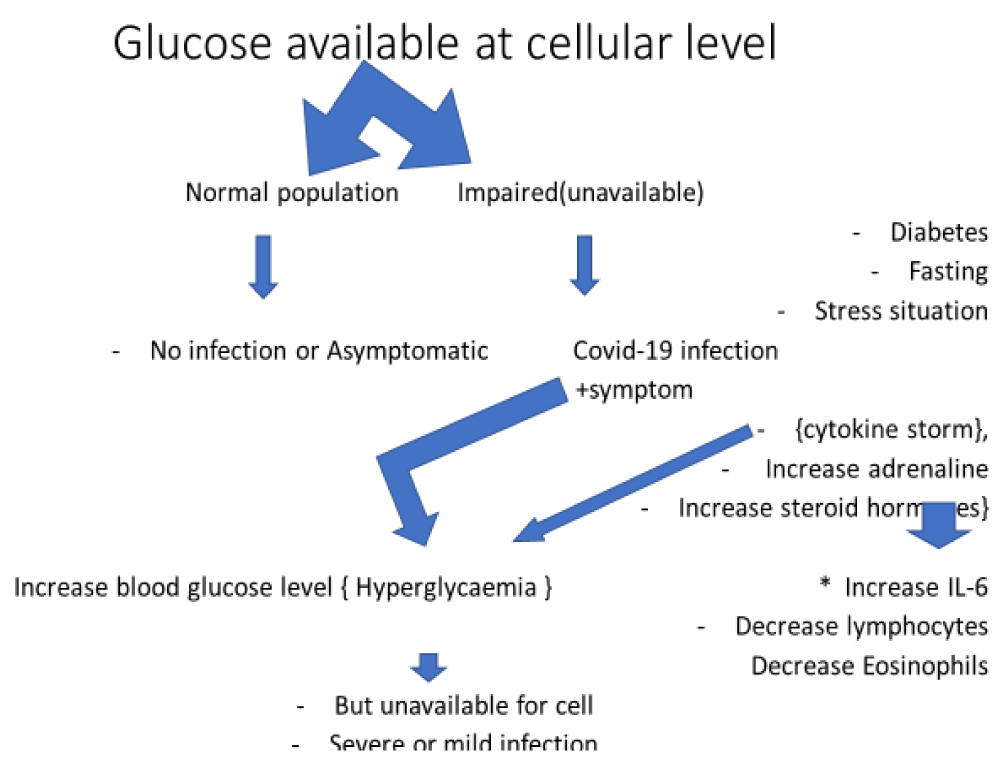
Glucose is a key player in COVID-19 pandemic
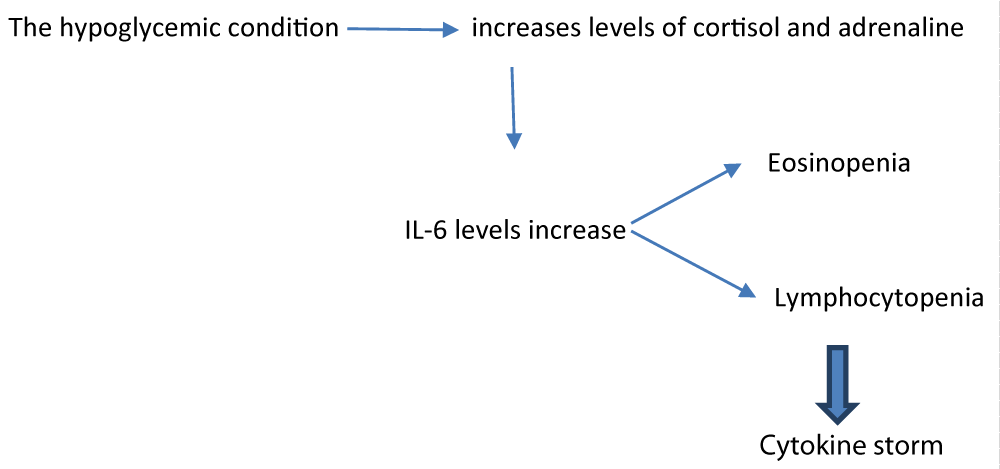
As seen in studies, COVID-19 infection is closely associated with glucose metabolism inside the cell. When seen in the population with normal glucose metabolism been infected by COVID-19 for them this remains a mild infection or they remain asymptomatic. But on the other hand, the case is not the same with the population having impaired/unavailable glucose metabolism this may be due to diabetes, prolonged fasting condition, stress situation, or obesity. In these cases, COVID-19 infection may take a serious look and can be fatal to a large extent. Generally, in impaired glucose metabolism in the body goes under stress conditions there occurs a cytokine storm phase in which hormonal changes occur like an increase in the level of adrenalin and an increase in steroid hormone (endogenous steroids).
These steroids have different actions on body functioning.
It increases blood glucose levels causing hyperglycemic conditions but which remains unavailable to cells causing the pre-diabetic stage.
They may also increase IL-6 levels in blood plasma. Decrease the level of lymphocytes and eosinophils causing lymphocytopenia and eosinopenia. These all-change results in severe COVID-19 infection.
The above observation has been an additional finding of the ongoing trial PISCOV (pH-based integrated SARS-CoV-2 immunity in the human subject), which is being done on 113 subjects and is a double-blind randomized intervention-controlled trial. The authors observed that the high-risk subject of both studies, as well as the control group, shares a common characteristic as a coherent which demonstrated the worsening, of COVID-19 syndrome in the above-mentioned categories having a common path-physiology if altered glucose availability to the cell.
Some studies were performed to assess cell glucose metabolism when there is a panic attack or anxiety. During a panic attack, there are significantly higher levels of glucose uptake by the cell but in case of glucose metabolism impairment or unavailability, glucose uptake by the cell became impaired which causes intracellular hypoglycemia. Severe hypoglycemia is associated with a marked curtailment of glucose in the cell and consumption of endogenous carbohydrate metabolites and amino acids leads to an excessive intracellular alkalosis of potential importance for the development of cell damage. This occurs as –
It was noticed that treating COVID-19 FLI cases with dexamethasone led to early improvement with non-progression to SARI. However, there could be a worsening of blood sugar control, particularly in diabetics, but the activation of the inflammatory pathway is prevented. The raised sugar levels can be easily controlled by and subsequently high insulin requirements.
• Those SARI cases who were euglycemic at the time of initial presentation recovered early and carried a good prognosis with less mortality as compared to those who were hyperglycaemic on presentation. Also, those FLI cases who maintained euglycemia or did not have any other risk factor which predisposes them to stress (Diabetes, Prolonged fasting, Obesity, major organ disorder, Physiological disorder, and Cancer) did not progress to SARI as the endogenous steroid secretion and sympathetic activation did not occur, the intracellular pH levels remained in the alkaline range. On the other hand, when an excess of lactate is produced from glucose via the anaerobic pathway, the pH becomes acidic and it favours virus entry in host cells and also the intracellular release of lysosomal enzymes. As for coronavirus to gain entry inside a human cell, the acidic environment of endosome is indispensable, and in subjects where the virus has entered the host cell, further replication leading to moderate to severe COVID-19 syndrome is facilitated by acidic intracellular and extracellular pH [19]. 10.18% of cases developed new-onset diabetes (total of 11 cases) out of which 10 were in COVID-19 this 19.2% incidence of new-onset diabetes in SARS-CoV-2 and prevalence of 26.9% in SARS-CoV-2, making total diabetes 46.1% in SARS-CoV-2, and out of all SARI cases, 26% of patients developed pulmonary fibrosis with consequent long-term complications. In these cases, COVID -19 infection may take a serious look and can be fatal. Generally in impaired glucose metabolism, the body undergoes stress response and there occurs a cytokine storm phase in which hormonal changes occur leading to an increase in levels of adrenalin, increase in steroid hormone (endogenous steroids), and Interleukin-6.
Of mortality in COVID-19 patients, it was seen only in diabetics SARS CoV-2 patients, thus were no death in non-diabetics in COVID-19.
1- The odds ratio of diabetic versus non-diabetic population developing COVID-19 is 4.19 with a relative risk of 1.33.
2- The association of Diabetics developing ARDS due to SARS-CoV-2 is significant. Out of 37 Diabetics, 24 were COVID-19 SARI (64.86%) there it was 8 Diabetics subjects who developed Bacterial pneumonia (21.6%), and 1 Diabetic developed Tuberculosis (2.7%). This is contrary to the major studies published earlier which show a negative correlation between Diabetes with ARDS [20,21]. However previous studies showing an association between Diabetes and ARDS were done on causations other than SARS-CoV-2, thus our observations on the association become unique.
3-Approximately 50% of SARI cases are non-COVID-19 and carry an equal or worse prognosis than COVID-19 and their treatment is well established with the curable outcome but is been ignored in the current pandemic.
4- Out of 37 Diabetics, 24 were COVID-19 SARI (64.86%) as compared to 76 non-diabetics, 28 developed COVID-19 SARI (36.8%). This is significant and has a bearing on the outcome of SARI also.
5- The deaths due to COVID-19 SARI were seen only in diabetics.
6- The association of dysregulated glucose metabolism and the proposed hypothesis as “Glucose a key player of COVID-19 Pandemic” is proved beyond doubt with the detailed explanation above as well as the observation of this SARI case series comparing the outcomes and associations of COVID-19 and SARI in diabetics v/s non-diabetics.
7-The finding of a new-onset of diabetics in COVID-19 SARI patients in 20% is explained by the dysregulated glucose metabolism under stressful conditions with the resultant diversion of glycolysis pathway and product pyruvate to an anaerobic pathway with increased production of lactate, as enzymatically heightened activity of lactate dehydrogenase, further resulting in increased glucose production by the liver through gluconeogenesis as well as glycogenolysis to regulated lactate levels in the blood. The findings of high levels of LDH, IL-6, and ferritin in COVID-19, and SARI cases are thus explained.
8- The authors further propose that the progression of FLI to SARI in COVID-19 is preventable in both diabetics as well as a non-diabetic population if the key player glucose is taken care of. And the measures are; to avoid prolonged fasting and stressful situation as this will stimulate the secretion of endogenous catecholamines and steroid hormones resulting in activation of the inflammatory pathway through Interleukins-6.
9- The role of low-dose dexamethasone in preventing the progression of mild flu-like illness to severe respiratory illness is explained by the fact that exogenous steroid prevents activation of the endogenous release of steroids and catecholamines with further chain reaction and activation of inflammatory pathways. However, this observation and its trial report as the PISCOV trial are due to be published soon.
Future directions
Our study highlights the impact of lifestyle disorders like Diabetes, Hypertension, Obesity, Major stress disorders, and various Cancers on the propagation and dissemination of infectious pandemics such as COVID-19. It also reveals that disorders like diabetes can be caused by an infective organism SARS-CoV-2, thus impelling us to put forth the hypothesis “Germ Theory of Diabetes”. Thus, we conclude that our observation and research be further continued on the lines where we prepare the ground for improving the global health and further prevention of such devastating pandemics by controlling the lifestyle disorders.
The age range of the population suffering most from SARI is 51-60 years in our case series of SARI cases. Further what intervention can be done as a protective measure in this particular age range to reduce morbidity and mortality will be our future direction.
Do initial interventions in the outpatient department (OPD) on a patient presenting as FLI could protect their progress to SARI and or sub-group complications, irrespective of the cause of FLI in a current scenario of global emergency. The impact of oral dexamethasone in a dose of 3 ml/day (adult) given to FLI cases in the OPD setting to see its impact on the progression or non-progression to a Severe Acute Respiratory Illness as compared to the controlled group who were not given dexamethasone will be our future direction based on the observations of this case series. This observation has been attempted from the finding which was seen in the Victoria trial.
The causes of SARI other than SARS-CoV-2 like tuberculosis and bacterial pneumonia carry more or equally bad prognosis with more morbidity and mortality than COVID-19 and must be studied further in a randomized controlled trial on a large number of cases.
Limitation of this study
The small number of cases is of course a limiting factor in this case series.
This case series is a purely observational study and is based on a COHORT group.
This SARI (Severe Acute Respiratory Illness) case series has been done as an observational study on a common COHORT group who presented in the ER of a tertiary care hospital during the COVID-19 pandemic in the city of Taj Mahal, Agra between 15 March to 30 October 2020. It has been attempted to know the causes of SARI to find out various other reasons for SARI presentation besides COVID-19 and which received less medical attention due to a focused global approach to tackle the pandemic. Establishing the cause-effect relationship between lifestyle disorders like Diabetes, Obesity, Hypertension, psychological problems on the rapidly spreading community infections like Tuberculosis, Community-acquired Pneumonias, and viral infections like SARS-CoV-2 is one of the main aims and objectives for which this study was undertaken. The various causes which are present as SARI, their clinical profile, epidemiology, management outcome, and mortality were analyzed and compared in this case series.
Out of 113 cases of SARI, 46% were due to COVID-19, followed by 23% of cases due to Tuberculosis and Bacterial pneumonia as 20% of cases. Death was seen more in males (8 out of 87) 9.1% than in females (1 out of 26) 3.8%. Thus, it points out that SARI is more fatal in males, irrespective of the cause. The mortality in COVID-19 patients is 3.8% (2 out of 52) with 5% mortality rates in males versus 0% in females. Thus, we see that COVID-19 carries a bad prognosis in males as compared to females.
The deaths in TB/Koch’s lung were (4 out of 26), about 15.3%. Thus, the mortality rate of TB/Koch’s Lung is maximum, followed by Bacterial Pneumonia, 8.6%, and then COVID-19, 3.8%. However, the COVID-19 tends to affect males more, both in infection and severity. Diabetes mellitus was the most common co-morbid condition associated with SARI patients (32.7%), followed by hypertension (10.6%) and heart disease (5.3%).
It can be appreciated that 10.18% of cases developed new-onset diabetes (a total of 11 cases) out of which 10 patients were in COVID-19. Thus 19.2% incidence of new-onset diabetes in SARS-CoV-2 and prevalence of pre-existing diabetes in 26.9% in SARS-CoV-2 patients. Making total diabetes 46.1% in SARS-COV-2. The association of diabetes with bacterial pneumonia was 34.7%. However, the finding of a new onset of diabetes in COVID-19 patients is a unique and significant observation and was persisting up to 3 months observation period after recovery from COVID-19. It was noticed while treating COVID-19 FLI cases, that those cases that were treated with dexamethasone led to early improvement with non-progression to SARI and prevention of consequent complications such as cytokine storm syndrome and multi-organ failure. The pathways of Glucose metabolism and how it affects the outcome of a simple viral flu presenting as an influenza-like illness to either complete cure or progression to a Severe Acute Respiratory Illness with activation of inflammatory pathways are explained in the study. In this study, we also raised concern about the growing association of an infectious pandemic with lifestyle disorders which are non-communicable diseases but carry with them the poten.
- Hatem A, Mohamed S, Abu Elhassan UE, Ismael EAM, Rizk MS, El-Kholy A, El-Harras M. Clinical characteristics and outcomes of patients with severe acute respiratory infections (SARI): results from the Egyptian surveillance study 2010-2014. Multidiscip Respir Med. 2019 Apr 1;14:11. doi: 10.1186/s40248-019-0174-7. PMID: 30976418; PMCID: PMC6442424.
- World Health Organization. Regional Office for Europe. Overview of sentinel systems for hospitalized severe acute respiratory infections (SARI) represented in the weekly Euro Flu surveillance bulletin 2013.
- World Health Organization. Regional Office for Europe. Overview of sentinel systems for hospitalized severe acute respiratory infections (SARI) represented in the weekly Euro Flu surveillance bulletin. 2013.
- Walaza S, Tempia S, Dreyer A, Dawood H, Variava E, Martinson NA, Moyes J, Cohen AL, Wolter N, von Mollendorf C, von Gottberg A, Haffejee S, Treurnicht F, Hellferscee O, Ismail N, Cohen C. The Burden and Clinical Presentation of Pulmonary Tuberculosis in Adults With Severe Respiratory Illness in a High Human Immunodeficiency Virus Prevalence Setting, 2012-2014. Open Forum Infect Dis. 2017 Aug 7;4(3):ofx116. doi: 10.1093/ofid/ofx116. PMID: 28852676; PMCID: PMC5570023.
- Tuberculosis. WHO.
- Rubino F. New-Onset Diabetes in Covid-19. Correspondence August 2020. N England Journal Med. 2020; 383:789-790.
- Chee YJ, Ng SJH, Yeoh E. Diabetic ketoacidosis precipitated by Covid-19 in a patient with newly diagnosed diabetes mellitus. Diabetes Res Clin Pract. 2020 Jun;164:108166. doi: 10.1016/j.diabres.2020.108166. Epub 2020 Apr 24. PMID: 32339533; PMCID: PMC7194589.
- Li J, Wang X, Chen J, Zuo X, Zhang H, Deng A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab. 2020 Oct;22(10):1935-1941. doi: 10.1111/dom.14057. Epub 2020 May 18. PMID: 32314455; PMCID: PMC7264681.
- Ren H, Yang Y, Wang F, Yan Y, Shi X, Dong K, Yu X, Zhang S. Association of the insulin resistance marker TyG index with the severity and mortality of COVID-19. Cardiovasc Diabetol. 2020 May 11;19(1):58. doi: 10.1186/s12933-020-01035-2. PMID: 32393351; PMCID: PMC7213552.
- Mallapaty S. Meet the scientists investigating the origins of the COVID pandemic. Nature. 2020 Dec;588(7837):208. doi: 10.1038/d41586-020-03402-1. PMID: 33262500.
- worldometer. United Nations, Statistics Division 761. doi:10.1164/rccm.200912-1918OC. World Health Organization. WHO surveillance case definitions for ILI and SARI. 2014 https://www. who.int/influenza/ surveillance monitoring/ili_ sari_ surveillance_case_definition/en/.
- World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected Interim guidance 13 March 2020 WHO Paper.
- Gupta N, Praharaj I, Bhatnagar T, Vivian Thangaraj JW, Giri S, Chauhan H, Kulkarni S, Murhekar M, Singh S, Gangakhedkar RR, Bhargava B; ICMR COVID Team. Severe acute respiratory illness surveillance for coronavirus disease 2019, India, 2020. Indian J Med Res. 2020 Feb & Mar;151(2 & 3):236-240. doi: 10.4103/ijmr.IJMR_1035_20. PMID: 32362647; PMCID: PMC7357403.
- Hatem A, Mohamed S, Abu Elhassan UE, Ismael EAM, Rizk MS, El-Kholy A, El-Harras M. Clinical characteristics and outcomes of patients with severe acute respiratory infections (SARI): results from the Egyptian surveillance study 2010-2014. Multidiscip Respir Med. 2019 Apr 1;14:11. doi: 10.1186/s40248-019-0174-7. PMID: 30976418; PMCID: PMC6442424.
- https://criticalcareblogspot.com/2020/12/10/hyperlactatemia-in-critical-illness-time-for-reappraisal/
- Revelly JP, Tappy L, Martinez A, Bollmann M, Cayeux MC, Berger MM, Chioléro RL. Lactate and glucose metabolism in severe sepsis and cardiogenic shock. Crit Care Med. 2005 Oct;33(10):2235-40. doi: 10.1097/01.ccm.0000181525.99295.8f. PMID: 16215376.
- Jansen TC, van Bommel J, Schoonderbeek FJ, Sleeswijk Visser SJ, van der Klooster JM, Lima AP, Willemsen SP, Bakker J; LACTATE study group. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010 Sep 15;182(6):752-61. doi: 10.1164/rccm.200912-1918OC. Epub 2010 May 12. PMID: 20463176.
- Al-Toum R, Bdour S, Ayyash H. Adenovirus Infections in Jordanian Hospitalized Paediatric Patients: Prevalence and Clinical Features. J Med J. 2009; 43(3):171–179.
- Pelligrino D. Journal of Cerebral Blood Flow and Metabolism 1:85-96 © 1981 Raven Press, New York Regulation of Extra- and Intracellular pH in the Brain in Severe Hypoglycemia.
- Boyle AJ. Identifying associations between diabetes and acute respiratory distress syndrome in patients with acute hypoxemic respiratory failure: an analysis of the LUNG SAFE database Critical Care. 2018; 22: 268.
- Yu S. (2013) Role of Diabetes in the Development of Acute Respiratory Distress Syndrome.
Crit Care Med. 2013 Dec; 41(12): 2720–2732.