More Information
Submitted: July 20, 2021 | Approved: August 09, 2021 | Published: August 10, 2021
How to cite this article: Bonaga B, Taravilla ERE, Carrilero-López C, Castillo-Lag MD, Boehm LM, et al. An educational strategy for the implementation of a delirium assessment tool. J Clin Intensive Care Med. 2021; 6: 015-020.
DOI: 10.29328/journal.jcicm.1001035
Copyright License: © 2021 Bonaga B, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
An educational strategy for the implementation of a delirium assessment tool
Beatriz Bonaga1*, Elena Ruiz-Escribano Taravilla2, Carmen Carrilero-López3, María Dolores Castillo-Lag3, Leanne M Boehm4, Ángela Prado Mira5, María Joaquina Piqueras Diaz6 and E Wesley Ely7
1Hospital Pharmacist, Hospital Clínico Universitario Lozano Blesa, Avenida San Juan Bosco 15, 50009 Zaragoza, Spain
2Intensivist, Intensive Care Unit, Complejo Hospitalario Universitario de Albacete, Spain
3Registered Nurse. Intensive Care Unit, Complejo Hospitalario Universitario de Albacete, Spain
4Department of Medicine, Division of Allergy, Pulmonary and Critical Care Medicine, Vanderbilt University, Nashville, TN, USA
5Intensivist, Intensive Care Unit, Complejo Hospitalario Universitario de Albacete, Spain
6Registered Nurse. Intensive Care Unit, Complejo Hospitalario Universitario de Albacete, Spain
7Veterans Affairs Clinical Science Research and Development Service, Geriatric Research, Education and Clinical Center, (GRECC), USA
*Address for Correspondence: Beatriz Bonaga, PhD, Hospital Pharmacist, Hospital Clínico Universitario Lozano Blesa, Avenida San Juan Bosco 15, 50009 Zaragoza, Spain, Tel: +34660427210; Email: [email protected]; [email protected]
Background: Delirium is an acute syndrome of organ dysfunction with long-term consequences which commonly occurs in the Intensive Care Unit (ICU). The incidence of delirium ranges from 30% - 50% in low severity ICU patients and up to 80% in mechanically ventilated patients. This condition is frequently under-recognized and daily routine screening is a key strategy to early intervention. The Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) and the Intensive Care Delirium Screening Checklist (ICDSC) are the most recommended assessment tools for detecting delirium in the critical ill patient.
Objective: The main objective of this study is to educate ICU staff about delirium. In addition, nurses were trained to use the CAM-ICU as a standard screening tool. The intervention was evaluated through a survey aimed at ICU staff.
Methods: An educational intervention was started in 2014 in our ICU. An educational package for ICU staff consisted of a didactic brochure and explanatory videos. One-on-one teaching, case based scenarios and didactic teaching were strategies used in the implementation process. The entire intervention was evaluated by means of a survey directed to the professionals.
Results: The structure of the didactic brochure was simple in order to have an easy understanding of the CAM-ICU tool. We also created 10-minute videos. According to the results of the satisfaction survey (N=62), disorganized thinking was the most difficult feature of CAM-ICU to interpret. When in doubt, consultation between co-workers was the primary resource selected by unit staff.
Conclusion: This initiative achieved the objective of training health care professionals in the application of the CAM-ICU tool with a good level of satisfaction from them. Therefore, ICU staff consider delirium management in the broader picture of critically ill patient care as a major activity of daily practice.
Delirium is a commonly observed pathology for adult patients in an Intensive Care Unit (ICU). This condition manifests as a rapidly developing disturbance of both consciousness and cognition which tends to fluctuate throughout the course of the day [1]. Delirium affects from 30% - 50% [2-4] to 80% in mechanically ventilated patients [5]. The consequences associated with delirium onset include prolonged mechanical ventilation, increased hospital length of stay, higher costs and mortality [6]. Furthermore, following discharge, the length of ICU delirium is correlated with the development of long-term cognitive dysfunction, physical disability and death up to one year later [1,7]. Given the negative consequences associated with delirium as well as its frequency, prevention is essential [8]. With a fluctuating nature of delirium symptoms, the bedside nurse is the ICU caregiver best suited to screen for delirium [9]. Research indicates that nurse manager and physician leadership played a large role in creating a supportive ICU environment [10].
Clinical practice guidelines for the management of pain, agitation and delirium recommend all adult ICU patients to be regularly assessed for delirium using either the Confusion Assessment Method for the ICU (CAM-ICU) or the Intensive Care Delirium Screening Checklist (ICDSC) [11-15]. Despite guideline recommendations, routine delirium assessments are not common practice in the ICU [8,16]; therefore, delirium is commonly overlooked [17]. A study showed 48% (n = 417) of the patients were monitored for symptoms of delirium; using a validated score in 27% (n = 234) [18].
The key to delirium detection in critically ill patients is the implementation and routine use of a validated, structured diagnostic tools [16,19]. The CAM-ICU and ICDSC have demonstrated how healthcare professionals can detect delirium more effectively [20].
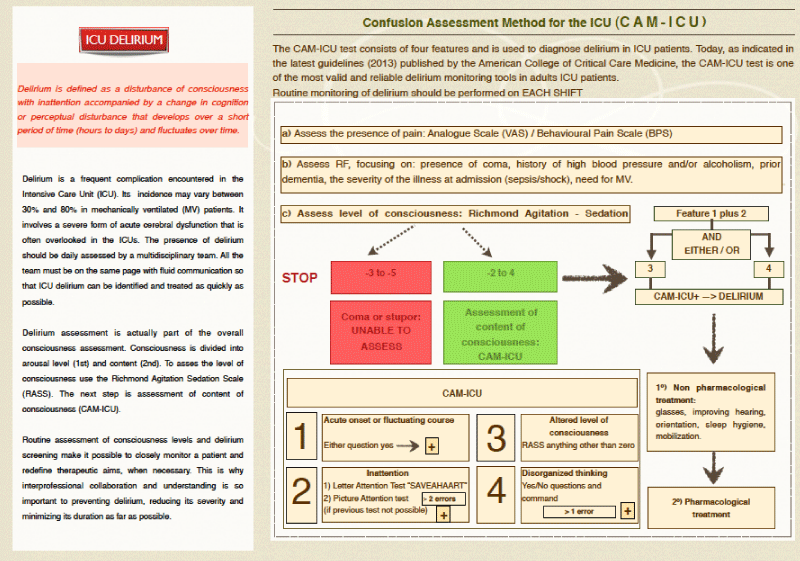
The CAM-ICU is a 4-part delirium screening tool used once per shift by nursing staff. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients include the CAM-ICU among the recommended tools for monitoring ICU delirium [10,11]. The CAM-ICU is valid and reliable, with 80% sensitivity and 96% specificity in patients receiving mechanical ventilation making it ideal for the ICU setting [10].
Education is essential for healthcare professionals to understand how to apply a tool to ensure that correct delirium assessment is performed. There is evidence suggesting that the lack of training for using the CAM-ICU is one of the main reasons for its low implementation. In a study carried out in 2008, 37% (n = 331) of nurses indicated not having received training on the application of the CAM-ICU scale [20], coinciding with two other publications. In the first of these, 69% (n = 52) [16] of the ICU nurses and in the second, 44% (n = 76) [21] of the healthcare professionals surveyed, indicated not having received prior training on delirium assessment. There is also evidence that supporting continuing education is key to reducing the incidence of this pathology [16]. As literature shows, results of inter-professional teamwork training program improves quality of observed team behaviours (p = 0,012) [22]. A recent study concludes that nurses viewed the CAM-ICU as easy to use after didactic and hands-on education. They also felt the tool was helpful for identifying patients at risk for delirium [10].
At that time, in our ICU we did not use any tool to accurately identify delirium in daily practice. Following guideline recommendations [10] we decided to use a validated one screening tool to detect ICU delirium. To reach our purpose we decided to carry on an educational intervention in our ICU.
The main objective of this study is to educate ICU staff about delirium, risk factors and its consequences. In addition, nurses were trained to use the CAM-ICU as a standard screening tool. Our aim was to prevent ICU delirium as a part of standard care of the critically ill patient. We also evaluated the knowledge, perceptions and satisfaction of ICU staff through a survey.
In order to carry out the educational intervention, a multidisciplinary team composed by an intensivist, several nurses and a pharmacist was created. The CAM-ICU was selected out of the current validated tools available for monitoring delirium in critically ill patents [11,12]. The team of experts were previously trained on delirium assessment using this tool. The training of the leading team took place by means of a bibliographical review on the topic and the collaborative solving of real cases of patients undergoing delirium. Thereby, the experts were capable of executing each part of the tool and had great knowledge on managing ICU delirium. In this sense, the team was responsible of the educational training.
The educational package for staff on the ICU consisted of a didactic brochure and explanatory videos made by themselves. The materials chosen to train ICU healthcare professionals in CAM-ICU application consisted of two different formats that could be easily accessed and distributed. We decided on the selected formats because they were easily obtained and spread among ICU staff. Moreover they were based on other implemented educational studies on ICU delirium [9,23].
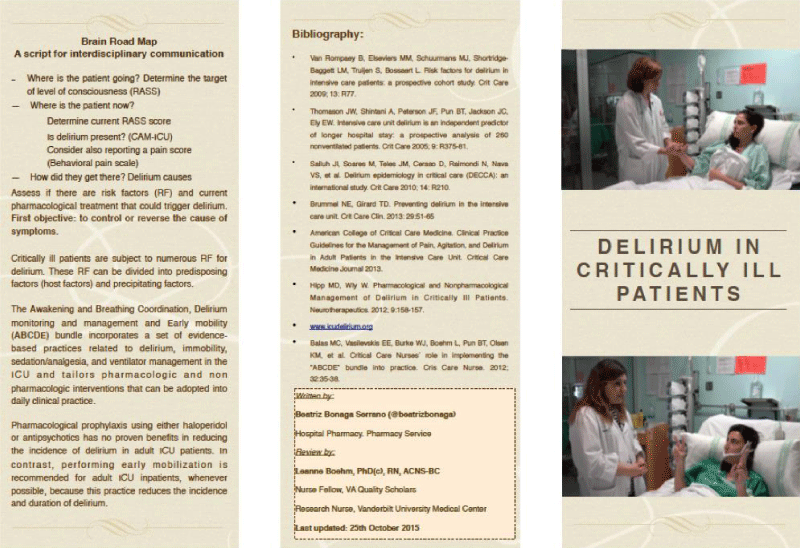
The materials consisted of an informative brochure complemented by the development of investigator-generated audio-visual material. The brochure was written by the ICU team of delirium experts in simple language with clear terminology in order to facilitate focal concepts to understand the application of the CAM-ICU tool. The brochure was reviewed by international ICU delirium experts and included the following sections (Figures 1,2):
Figure 1: Didactic brochure (part 1).
Figure 2: Didactic brochure (part 1).
A. Introduction: understanding the definition of delirium and its incidence rate
B. Explanation of the CAM-ICU as a validated tool for the diagnosis of delirium in critically ill patients. This tool comprises four features [12]:
1. Acute change or fluctuation in mental status in the last 24 hours
2. Inattention
3. Altered level of consciousness
4. Disorganized thinking
Steps to screening delirium in critically ill patients. To be diagnosed as delirious, the patient needs to show an acute change or fluctuation in mental status in the last 24 hours (Feature 1), accompanied by inattention (Feature 2), and either altered level of consciousness (Feature 3) or disorganized thinking (Feature 4) [12].
To develop the educational videos (http://bit.ly/1LJmo6z), the entire team along with a nurse simulating a patient participated. Each one of the scales for assessing analgesia, sedation and delirium in critically ill patients were presented. Along with this, a preliminary theoretical exposition was performed. Short videos (approximately 10 minutes), in which theoretical and practical approaches are combined. The theoretical area consists of a slide presentation detailing the key theoretical concepts in the detection of delirium using the CAM-ICU. The practical area covers each component comprising the scale, while its correct execution is explained.
Personal and individualized training was also provided to healthcare professionals regarding the application of the CAM-ICU scale. The educational program was provided to ICU staff by the multidisciplinary ICU team of experts in the delirium field. From April to October 2014, a pharmacist and an intensivist provided didactic teaching theory on delirium screening every morning shift. In addition, the CAM-ICU was executed in-situ, as a bedside demonstration, with the team responsible for the patient. With a view of making the percentage of monitoring known, the results obtained after the application of CAM-ICU were registered. Daily one-on-one teaching was provided by delirium champions.
Case-based scenarios presented by the team of experts were used to reinforce delirium concepts learned over time. Any doubts and questions in handling cases of delirium which arose were resolved by a delirium team of experts. As a follow-up to the training, monthly staff meetings were held along the next six months. New staff were trained and refresher training was provided to current staff members.
After the six-month educational period, a survey was conducted with physicians, nurses, and nurse assistants to assess level of satisfaction with the training received. For collecting data, we developed a 5- item questionnaire. Participation was anonymous and the data included demographic variables such as gender, age and professional category. The five questions included are indicated in Table 1.
| Table 1: Responses obtained in the questionnaire. | |||||
| After applying CAM-ICU, which is the most difficult feature to asses? | |||||
| Fluctuation | Inattention | Disorganized thinking | Altered level of onsciousness | n/a | |
| Physician (n = 11) | 9,0% | 27,3% | 54,6% | 9,1% | 0% |
| Nurse (n = 34) | 28,6% | 22,8% | 42,9% | 0% | 5,7% |
| Nurse assistant (n = 17) | 23,5% | 5,9% | 43,7% | 11,8% | 15,1% |
| How is your satisfaction with the received delirium training? State from 0 to 4. | |||||
| 0. Nule | 1. Scarce | 2. Appropriateness | 3. Good | 4. Excellent | |
| Physician (n = 11) | 0% | 0% | 18,2% | 63,6% | 18,2% |
| Nurse (n = 34) | 0% | 3,0% | 53,0% | 29,4% | 14,6% |
| Nurse assistant (n = 17) | 0% | 5,9% | 47,0% | 35,3% | 11,8% |
| Do you consider yourself properly trained in the delirium assessment? | |||||
| Yes | No | n/a | |||
| Physician (n = 11) | 54,5% | 36,4% | 9,1% | ||
| Nurse (n = 34) | 76,5% | 23,5% | 0% | ||
| Nurse assistant (n = 17) | 35,3% | 64,7% | 0% | ||
| In case of doubt, which is your main resource to consult? | |||||
| Workmate | Educational material | Don´t apply the scale | Other | n/a | |
| Physician (n = 11) | 53,8% | 30,8% | 15,4% | 0% | 0% |
| Nurse (n = 34) | 71,0% | 21,0% | 5,3% | 2,7% | - |
| Nurse assistant (n = 17) | 88,2% | 11,8% | 0% | 0% | - |
| Which is the part of the educational intervention you like the most? | |||||
| Educational meetings | Training videos | Brochure | Individualized training | None of them | |
| Physician (n = 11) | 50,0% | 33,3% | 0% | 8,4% | 8,3% |
| Nurse (n = 34) | 8,4% | 37,8% | 11,1% | 22,2% | 4,5% |
| Nurse assistant (n = 17) | 36,8% | 52,6% | 5,3% | 5,3% | 0% |
| n/a: no answer. | |||||
All questions were multiple-choice type, and in the event that more than one option was indicated, all responses were considered.
With regards to the satisfaction survey, a total of 62 responses were obtained, with a total participation percentage of 100%. Participants demographics are described in Table 2. The majority of respondents were nurses (54.8%; n = 34) with predominant age ranging from 40-50 years (64.7% of them). Table 1 indicates the responses obtained for each of the questions formulated classified by groups. All the respondents reported disorganized thinking as the most difficult part to assess delirium. Regarding satisfaction with education, the majority of nurses reported satisfaction as appropriate and doctors as good. In this sense, they considered themselves well trained and the workmate was the main consulted resource when assessment findings were unclear or difficult to interpret. For the doctors, educational meetings were the best resource implemented. On the other hand, training videos were the best educational resource for nurses.
| Table 2: Participant Demographics (n = 62). | |||||
| Age | |||||
| 20-30 years | 30-40 years | 40-50 years | 50-60 years | n/a | |
| Physician (n = 11) | 27,3% | 18,2% | 18,2% | 36,3% | 0,0 % |
| Nurse (n = 34) | 11,8% | 14,7% | 64,7% | 5,8% | 3,0 % |
| Nurse assistant (n = 17) | 0,0% | 0,0% | 94,1% | 5,9% | 0,0 % |
| Gender | |||||
| Male | Female | ||||
| Physician (n = 11) | 45,4% | 8,8% | |||
| Nurse (n = 34) | 54,6% | 91,2% | |||
| Nurse assistant (n = 17) | 0,0% | 100,0% | |||
| n/a: no answer | |||||
Routine delirium monitoring may facilitate prevention and improve delirium management in critically ill patients. Thereby, improving the quality of care of critically ill patients. As previously indicated, lack of training may be a significant barrier in the detection of delirium. Accordingly, we made attempts to mitigate under recognition through the implementation of multidisciplinary CAM-ICU screening using educational videos and an ICU delirium didactic brochure. Application of the CAM-ICU by the multidisciplinary ICU team was simple and took only a few minutes to implement9. Additionally, more than half of the healthcare professionals considered the CAM-ICU training as good or excellent and a majority indicated they were suitably trained to detect delirium using the CAM-ICU (54.5% doctors and 76.5% nurses). Conversely, the most complicated CAM-ICU features to interpret were disorganized thinking (Feature 4) and acute fluctuation of changes in mental state (Feature 1). In the event of uncertainty, the majority of healthcare professionals consulted their co-workers.
Several studies have described educational interventions carried out with this same objective [10]. First, a 74% reduction of incident delirium was reported following an educational intervention that consisted of one educational session describing the general concepts of the CAM-ICU tool (5 minutes) and the importance of the correct CAM-ICU application (5 minutes) [24]. Another study reported an increase in delirium assessment from 30% to 95% through the identification and correction of assessment barriers [25]. In this study, nursing staff were trained using educational videos representing different clinical situations to facilitate implementation of the delirium screening tool. Thirdly, an educational strategy consisting of 20-minute case study reviews along with monthly individual educational sessions and interventions with a delirium expert improved the detection of delirium by 84% [26]. Lastly, a four-week online training program followed by a 10-week monitoring period in which several expert nurses were in charge of training their co-workers resulted in an 84% (849 of 1011) of CAM-ICU assessment [27]. A study shows how an e-learning tool improved healthcare workers’ delirium recognition and knowledge [27].
Delirium screening has not become common practice due to the complexity of applying the scale, assessment burden [7,20], and lack of training [16]. However, by using validated tools and multifaceted staff training, monitoring delirium can be integrated into daily clinical practice. There are several strategies suggested for the implementation of delirium assessment [6]. Highlights for our result included a multi-faceted approach to implement a validated tool.
We chose our specific method because as literature demonstrates a resultant improvement in delirium assessment by ICU staff, especially with bedside nurses9, has turned to be relevant to clinical practice.
Some limitations need to be considered in our study. The sample size is small and may need to be larger to reproduce the obtained results. It could also be interesting to design a pre/post study to assess the real impact of the ICU delirium education intervention. It would also be important to include objective tools to evaluate how knowledge and skills improve for ICU staff during the study. Another limitation inherent to survey methods is the possibility of responder bias regarding the participants of the study. However, we did have 100% participation in our survey, thus reducing the impact of this limitation. Another limitation in our study is that before implementing the educational intervention, delirium was not monitored, hence the efficacy of the educational intervention cannot be compared in terms of increase in monitoring. Moreover, the study has important strengths. We utilized a validated and recommended instrument to assess delirium in our critically ill patients. Additionally, after implementation of the educational program, we noted improvements in delirium management in the critically ill patients. The use of educational resources suchlike brochure, videos or the individualized educational intervention may allow the level of awareness in healthcare professionals to increase regarding the relevance of monitoring the presence of delirium in critical patients.
With the intervention carried out, we have achieved the objective of training professionals in the management of delirium in critically ill patients. Especially important aspect given the negative consequences that this pathology can have. All this allows us to act in advance, thus preventing the possible effects that may appear and improving the care of our patients.
Our educational intervention prepared ICU staff for the proper screening and the treatment of delirium in critically ill patients. In this sense, a well-trained multidisciplinary team therefore plays a key role in the identification and management of delirium, mainly through inter-professional communication.
Our initiative achieves the fundamental objective of training healthcare professionals in the application of the CAM-ICU, thereby improving the diagnosis of delirium in critically ill patients. Most nurses felt the well prepared to identify patients at risk for delirium.
The educational methodology has received positive feedback by ICU staff.
Since we started educational intervention, the CAM-ICU has been successfully implemented in the daily nursing workflow. We want to continue working in this line and study its impact over the years. In our case, this project has been the starting point to learn to manage delirium. Our model could serve other professionals to improve the quality of care for their patients.
- Brummel NE, Girard TD. Preventing delirium in the intensive care unit. Crit Care Clin. 2013; 29: 51-65. PubMed: https://pubmed.ncbi.nlm.nih.gov/23182527/
- Van Rompaey B, Elseviers MM, Schuurmans MJ, Shortridge – Baggett LM, Truijen S, et al. Risks factors for delirium in intensive care patients: a prospective cohort study. Crit Care. 2009; 13: R77. PubMed: https://pubmed.ncbi.nlm.nih.gov/19457226/
- Thomason JW, Shintani A, Peterson JF, Pun BT, Jackson JC, et al. Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit Care. 2005; 9: 375-381. PubMed: https://pubmed.ncbi.nlm.nih.gov/16137350/
- Salluh JI, Soares M, Teles JM, Ceraso D, Raimondi N, et al. Delirium Epidemiology in Critical Care Study Group. Delirium epidemiology in critical care (DECCA): an international study. Crit Care. 2010; 14: R210. PubMed: https://pubmed.ncbi.nlm.nih.gov/21092264/
- Ely W, Shintani A, Truman B, Speroff T, Gordon SM, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004; 291: 1753-1762. PubMed: https://pubmed.ncbi.nlm.nih.gov/15082703/
- Brummel NE, Vasilevskis EE, Han JH, Boehm L, Pun BT, et al. Implemeting delirium screening in the UCI: secrets to success. Crit Care Med. 2013; 41: 2196-2208. PubMed: https://pubmed.ncbi.nlm.nih.gov/23896832/
- Guenther MD, Popp J, Koecher L, Muders T, Wrigge H, et al. Validity and reliability of the CAM-ICU flowsheet to diagnose delirium in surgical ICU patients. J Crit Care. 2010; 25: 144-151. PubMed: https://pubmed.ncbi.nlm.nih.gov/19828283/
- Van Rompaey B, Elseviers MM, Schuurmans MJ, Shortridge-Baggett LM, Truijen S, et al. Risk factors for delirium in intensive care patients: a prospective cohort study. Crit Care. 2009; 13: R77. PubMed: https://pubmed.ncbi.nlm.nih.gov/19457226/
- Dewlin JW, Marquis F, Riker RR, Robbins T, Garpestad E, et al. Combined didactic and scenario-based education improves the ability of intensive care unit staff to recognize delirium at the bedside. Crit Care. 2008; 12: R19. PubMed: https://pubmed.ncbi.nlm.nih.gov/18291021/
- Boehm LM, Pun BT, Stollings JL, Girard TD, Rock P, et al. A multisite study of nurse-reported perceptions and practice of ABCDEF bundle components. Intensive Crit Care Nurs. 2020; 60: 102872. PubMed: https://pubmed.ncbi.nlm.nih.gov/32389395/
- Barr J, Fraser GL, Puntillo K et al. American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013; 41: 263-306. PubMed: https://pubmed.ncbi.nlm.nih.gov/23269131/
- Ely EW, Margolin R, Francis J, Ely EW, Gélinas C, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assesment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med. 2001; 29: 1370-1379. PubMed: https://pubmed.ncbi.nlm.nih.gov/11445689/
- Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screnning Checklist: evaluation of a new screening tool. Intensive Care Med. 2001; 27: 859-864. PubMed: https://pubmed.ncbi.nlm.nih.gov/11430542/
- Chen TJ, Chung YW, Chang HR, Chen PY, Wu CR, et al. Diagnostic accuracy of the CAM-ICU and ICDSC in detecting intensive care unit delirium: A bivariate meta-analysis. Int J Nurs Stud. 2021; 113: 103782. PubMed: https://pubmed.ncbi.nlm.nih.gov/33120134/
- Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018; 46: e825–e873. PubMed: https://pubmed.ncbi.nlm.nih.gov/30113379/
- Christensen M. An exploratory study of staff nurses ́ knowledge of delirium in the medical ICU: an Asian perspective. Intensive Crit Care Nurs. 2014; 30: 54-60. PubMed: https://pubmed.ncbi.nlm.nih.gov/24042089/
- Boot R. Delirium: a review of the nurses role in the intensive care unit. Intensive Crit Care Nurs. 2012; 28: 185-189. PubMed: https://pubmed.ncbi.nlm.nih.gov/22245104/
- Luetz A, Balzer F, Radtke FM, Jones C, Citerio G, et al. Delirium, sedation and analgesia in the Intensive Care Unit: a multinational, two part survey among intensivists. PLoS One. 2014; 9: e11935. PubMed: https://pubmed.ncbi.nlm.nih.gov/25398099/
- Page VJ, Navarange S, Gama S, McAuley DF. Routine delirium monitoring in a UK critical care unit. Crit Care Med. 2009; 13: R16. PubMed: https://pubmed.ncbi.nlm.nih.gov/19203391/
- Devlin JW, Fong JJ, Howard EP, Skrobik Y, McCoy N, et al. Assesment of delirium in the intensive care unit: nursing practices and perceptions. Am J Crit Care. 2008; 17: 555-565. PubMed: https://pubmed.ncbi.nlm.nih.gov/18978240/
- Elliot SR. ICU Delirium: A Survey into nursing and medical staff knowledge of current practices and perceived barriers towards ICU delirium in the intensive care unit. Intensive Crit Care Nurs. 2014; 30: 333-338. PubMed: https://pubmed.ncbi.nlm.nih.gov/25201699/
- Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and health care outcomes (update). Cochrane Database Syst Rev. 2013; 28: CD002213. PubMed: https://pubmed.ncbi.nlm.nih.gov/23543515/
- Marino J, Bucher D, Beach M, Yegneswaran B, Cooper B. Implementation of an Intensive Care Unit Delirium Protocol: An interdisciplinary quality improvement project. Crit Care Nurse. 2015; 34: 273-284. PubMed: https://pubmed.ncbi.nlm.nih.gov/26244242/
- Swan JT. Decreasing inappropriate unable-to-assess ratings for the confusion assessment method for the intensive care unit. Am J Crit Care. 2014; 23: 60-69. PubMed: https://pubmed.ncbi.nlm.nih.gov/24382618/
- Riekerk B, Pen EJ, Hofhuis JG, Rommes JH, Schultz MJ, et al. Limitations and practicalities of CAM-ICU implementation, a delirium scoring system, in a Dutch intensive care unit. Intensive Crit Care Nurs. 2009; 25: 242-249. PubMed: https://pubmed.ncbi.nlm.nih.gov/19540761/
- Pun BT, Gordon SM, Peterson JF, Shintani AK, Jackson JC, et al. Large – scale implementation of sedation and delirium monitoring in the intensive care unit: a report from two medical centres. Crit Care Med. 2005; 33: 1199-2205. PubMed: https://pubmed.ncbi.nlm.nih.gov/15942331/
- Soja SL, Pandharipande PP, Fleming SB, Cotton BA, Miller LR, et al. Implementation, reliability testing, and compliance monitoring of the Confusion Assessment method for the Intensive Care Unit in trauma patients. Intensive Care Med. 2008; 34: 1263-1268. PubMed: https://pubmed.ncbi.nlm.nih.gov/18297270/
- Detroyer E, Dobbels F, Debonnaire D, Irving K, Teodorczuk A, et al. The effect of an interactive delirium e-learning tool on healthcare workers´ delirium recognition, knowledge, and strain in caring for delirious patients: a pilot pre-test/post-test study. BMC Med Educ. 2016; 16: 17. PubMed: https://pubmed.ncbi.nlm.nih.gov/26768589/